Always here
when you need us
Our care offers conversation & companionship to combat loneliness through the winter months.
As we get older, we become more prone to the risk of falls possibly due to increased frailty, medication or other age related conditions. Falls are one of the most common causes of injury in elderly people1, with around 30% of adults aged over 65 in England experiencing at least one fall per year.2 While many falls result in only minor bruising, some can cause serious life threatening injuries. The challenge? Symptoms don’t always appear immediately – some injuries may not present themselves for hours or even days after a fall.
This guide will help you identify both immediate and delayed symptoms to look for after an elderly person falls, so you know when to seek medical care.
Medical disclaimer: This guide is for informational purposes only and does not constitute medical advice. Always consult with a qualified healthcare professional for medical concerns. If you believe someone has a medical emergency, call emergency services immediately.
If you’re concerned about an older person having a fall accident, you can read our guide on falls prevention for elderly people. You may also find they’ll benefit from the support of a Home Care Assistant. A Home Carer can provide emotional support, as well as help with tidying and decluttering the home to reduce hazards that could cause future falls.
If your loved one has recently had a fall and you’re concerned about their wellbeing, our Convalescent Care service can help. A trained Care Assistant will visit your loved one at home to assist with an injury. They offer valuable support during recovery and are professionally trained to monitor your loved one and notice changes in their health or wellbeing.
To learn more about our services and how we can help, find your local Alina Homecare Team.

Anyone can have a fall, but falls in older adults are more common.3 There are a few reasons for this:
Around one third of people aged 65 and over, and over half of people aged 80 and over, will fall at least once a year.4 An increased risk of falls occurs in older individuals due to the natural ageing process. Ageing can result in muscle weakness and balance problems, vision loss, long term health conditions, or low blood pressure which can lead to dizziness.
Another consequence of ageing is the potential onset of osteoporosis. This is a health condition that weakens bones, causing them to become fragile and more likely to break. Fragility as a result of osteoporosis can lead to an increase in a person’s risk of falling, which could subsequently result in broken bones.
It’s estimated that over three million people in the UK have osteoporosis5, and it’s more commonly developed in older women than men.6 This is because of the female anatomy – ovaries produce oestrogen which helps protect bones. Following menopause, women lose bone density due to hormonal changes and the reduced production of oestrogen.7
Deficiencies such as having low levels of vitamin D in the body can also increase the chance of falls. This is because vitamin D deficiencies cause a drop in bone mineral density8 and therefore bone strength, increasing instability and the risk of a fall.
Falls can also be a consequence of various external risk factors, but most commonly arise from the following:
Slips and falls in the elderly are often preventable, yet research suggests that 10% of falls in people aged 75-79 result in a hospital visit, and this doubles to 20% for people aged 80 and over.9 Therefore, it’s important to try reducing the risk of falls to maintain health, confidence and independence in older people.
If your elderly loved one has had a fall injury that resulted in hospitalisation, they could benefit from our After Hospital Care. Being discharged from hospital, where they were receiving round the clock support, and readjusting to living independently at home can be unnerving. Our Home Carers can help with the transition and support your loved one to regain their confidence.
Some simple measures that you can implement for preventing a fall risk at home are:
Whilst they cannot rule out falls in older people, there are ways of monitoring elderly parents remotely to assist their safety and offer peace of mind for family members.
A personal alarm for the elderly can provide an instant alert should a fall occur. These are devices that can be worn around the neck or wrist and, when activated, will alert emergency services. Grab bars or pull cords can also be installed in bathrooms where falls are more likely to happen due to slippery surfaces.

If you’re present when an elderly loved one has a fall, stay calm and avoid panicking. You’ll need to determine the cause and whether there are any serious injuries from a fall.
After a fall, it’s important to wait until the shock of the fall has subsided before you try to move your loved one. Check your surroundings to ensure it’s safe for you to help them without causing injury to yourself. Only move them if you’re confident it’s safe to do so without making the situation or injuries worse. Moving them too soon could worsen injuries which may extend recovery time and lead to more serious consequences. It’s always best to first consult medical professionals, such as calling the emergency services.
If your loved one hit their head or lost consciousness when they fell, they may have sustained a head injury. In this case, you should call an ambulance immediately and avoid moving them. This is also relevant if you’re concerned about a potential sprain, fracture or broken bone. It’s advised that you leave them where they fell and wait for medical assistance to arrive.
In the event of an elderly person falling and an ambulance being called, make sure they’re as comfortable as possible whilst waiting for the ambulance to arrive. Cover them with blankets to keep them warm and dry (if outside) and make sure they drink plenty of fluids to stay hydrated, if it’s safe to do so.
In the aftermath of a fall, you may find an elderly loved one lacks confidence and becomes withdrawn; this may be because they feel as though they’ve lost their independence. If they’re able, encourage them to get back to daily routines and activities as soon as possible.
While an elderly person may not initially appear to be injured after a fall, it’s important to closely monitor them afterwards for signs of serious concerns. Sometimes symptoms are delayed and will present themselves gradually over time, so it’s valuable to be aware of different symptoms to look for after a fall.
Some immediate symptoms to look for after a fall are:
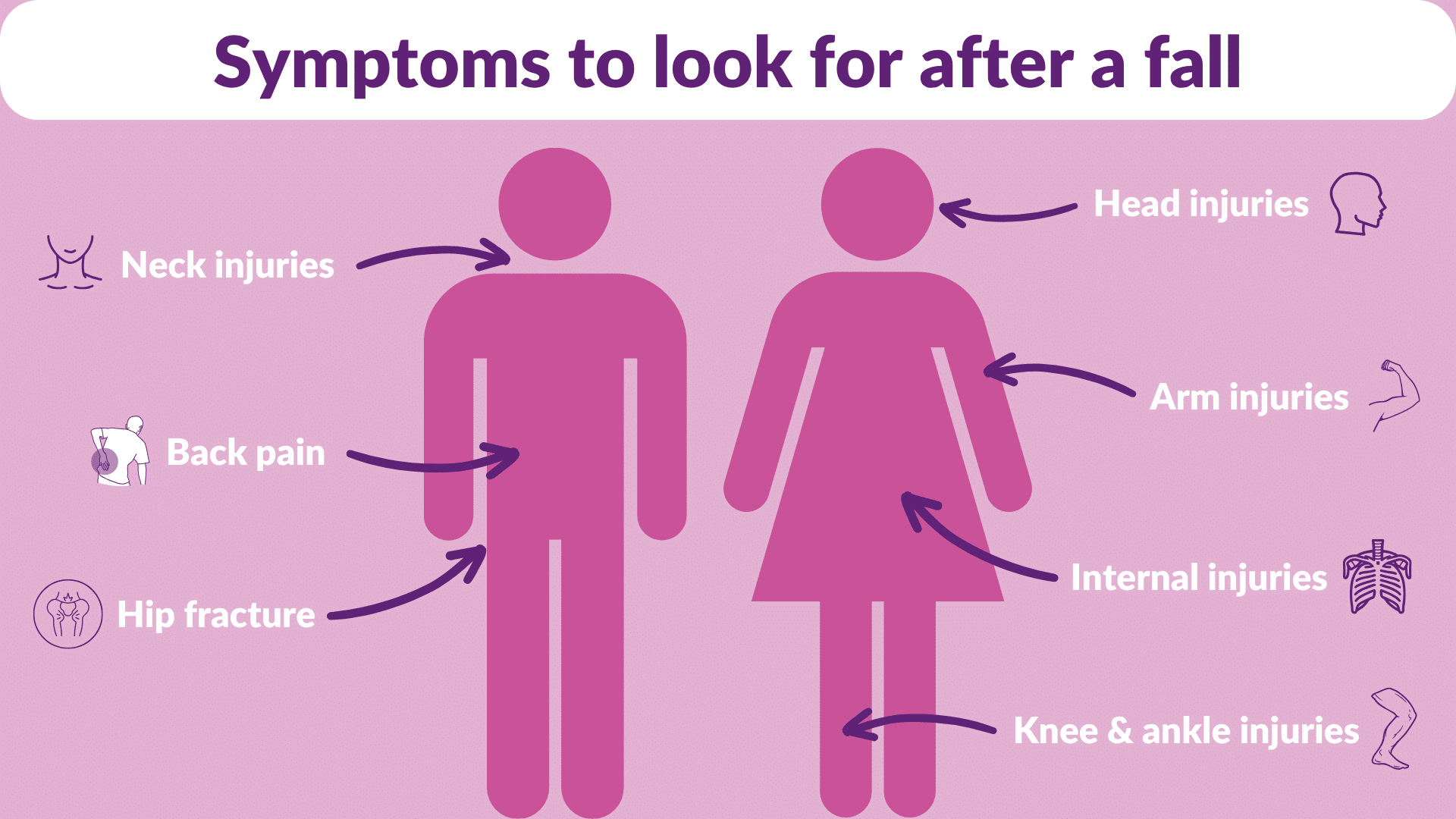
Following a fall, temporary pain may occur immediately. This pain may be short term or it could be more serious and require long term treatment. Read on to learn more about the most common injuries and symptoms to look for after a fall:
Bones weaken as we age, which means elderly people are more susceptible to broken bones after a fall. Broken bones in the arms or legs are easier to notice than internal breakages, such as the ribcage or hips. This is why it’s especially important to pay attention to any new pain that’s experienced after elderly people fall.
Pay close attention to symptoms that could indicate a broken bone; this could be pain when coughing or laughing, which may suggest a broken ribcage. Likewise, pain when moving or restricting walking could suggest a broken hip. If they experience new pain in areas where bones are likely to be broken, you should seek medical help from a trained professional to check this.
Often, when someone has a bump or fall, this can cause substantial bruising. This indicates there are broken blood vessels under the skin. Bruising can also imply more severe injuries, including sprains, strains or internal bleeding.
Due to thinner skin and fragile blood vessels beneath the surface, elderly skin is more prone to bruising. Therefore, elderly people are more likely to experience bruising after a fall. If the bruising is significant and painful and covers a large area, you should seek medical advice to determine if it requires attention.
Depending on the surroundings and the cause of a fall, an elderly person may have encountered sharp objects, such as gravel or stones, which could lead to cuts or skin lacerations. Serious cuts or lacerations may require medical intervention and stitches to stop the bleeding. If a laceration is deep enough, it could cause muscle, nerve or soft tissue damage. Prompt medical treatment can reduce the risk of infection, help reduce scarring and encourage faster healing.
After a fall or any impact with the ground, it’s normal to experience soreness and stiffness. Stiffness should usually subside quickly with stretching and moving around following a fall. However, if the pain or stiffness restricts the ability to move then it could be something serious. Serious injuries such as broken bones or spinal injuries can make it difficult to move immediately after a fall. If you notice unusual mobility limitations following an elderly fall, seek advice from a medical professional.
Losing balance and hitting the ground unexpectedly can result in immediate feelings of shock and pain. Sometimes, the initial pain may be minor and will subside or heal quickly. However, other times the pain can be more severe and ongoing.
If your elderly loved one experiences delayed soreness after a fall, this could be because of something more serious like a broken bone, sprain or muscular injury. Delayed pain can often occur after the shock and adrenaline of the fall have worn off.
Ignoring ongoing pain can result in the injury becoming worse over time and prolonging the healing process. It’s always recommended to seek medical attention after an elderly person falls to ensure they have no underlying injuries.
Similar to ongoing pain, sudden and sharp pains can also be an indication that there are serious injuries. Broken bones often involve sudden, sharp pain. In some cases, even the lightest pressure or movement of an injury can cause pain.
Not all injuries or symptoms are visible. If sudden, sharp pain is experienced then it’s possible there’s a serious injury and you should seek medical attention.
Swelling can often occur immediately after a fall and indicate there may be an injury. Swelling usually appears when there’s a broken bone, sprain or strain. However, you may not notice swelling straight after the fall has occurred. Instead, the swelling may increase throughout the day, so it’s an important symptom to look for after a fall.
If an elderly person has existing swollen limbs, this can make swelling after a fall difficult to notice. Swelling in seniors could be the result of water retention in the body. This is known as oedema and causes the legs and ankles to swell, but there are different kinds of exercises to reduce swollen ankles. If an elderly person experiences ankle swelling after a fall, you should consult a medical professional before attempting any exercises as there could be an underlying injury.
Internal injuries are among the most dangerous consequences of a fall because they’re not always immediately obvious. Unlike a broken bone or visible bruise, internal damage or bleeding is hidden from view, yet potentially life threatening. Falls can cause blunt force trauma to the abdomen, resulting in torn blood vessels, ruptured organs or internal bleeding.
Internal injury signs include:
If your loved one is taking blood thinning medication, they’re at higher risk of internal bleeding after a fall; therefore, even seemingly minor falls should be reported to a medical professional.
As well as the symptoms mentioned above, there are body injuries which you should be mindful of and pay close attention to. If you’re concerned about any of these in an elderly person after a fall, refer to the NHS website or seek professional medical advice.
If an elderly person hits their head during a fall or loses consciousness, you should seek medical attention immediately. Some signs of a head injury are not instantly obvious and will only present themselves later.
Signs of a head injury vary depending on the severity, but some common symptoms to look for after a fall are:
Whiplash is a common neck injury from falling. This type of injury is caused by a sudden, rapid movement of the head and neck. The sudden movement can cause a sprain in the soft neck tissue, resulting in neck pain, stiffness, headaches or dizziness. In some cases, the symptoms of whiplash may only appear several hours or days after the fall. The NHS recommends taking pain medication to help with the pain of whiplash and continuing with daily activities as normal to speed up recovery.11
It’s human instinct to brace ourselves for a fall – usually, this involves putting a hand or arm out to cushion the fall to the ground. This can lead to various arm injuries from falling in the elbows, shoulders or wrists. Minor injuries may heal on their own over time, while others may require medical intervention, such as a dislocation.
Back pain can often occur after a fall due to the sudden impact of hitting the ground. If an elderly person has existing back injuries, this can worsen the issue. However, back pain following a fall could be due to a serious injury such as a herniated disc or compression fracture.
Older adults with osteoporosis are at higher risk of experiencing compression fractures. Symptoms can include severe back pain and difficulty standing or walking. If you suspect an elderly person has back pain following a fall, they should get plenty of rest and consult a medical professional if the pain persists.
Hip fractures are one of the most serious consequences of elderly falls; around 76,000 hip fractures occur annually in the UK.12 They’re particularly common in elderly people and those with osteoporosis.
A broken hip is a serious injury and can take several weeks or months to recover from; it needs to be treated in hospital immediately.13 Warning signs of a hip fracture to look out for are:
Knee injuries from falling can be as minor as a bruise or sprain to a serious injury like a torn ligament or fracture. A sprain occurs when a ligament in the knee is overstretched and can usually be treat at home. A torn ligament, on the other hand, is considered a serious injury and often requires surgery to repair. Without proper treatment, a torn ligament can lead to chronic pain and further complications.
Knee pain after a fall usually signifies something serious if there’s significant swelling, severe pain or difficulty standing or walking. In this case, you should seek medical attention.
If an elderly person experiences knee or ankle swelling after a fall, you should always seek medical advice to ensure they receive the best treatment. However, the NHS does recommend using the PRICE method to help with swelling and supporting an injury for the first few days.14
Swelling often doesn’t appear immediately in ankle injuries and could take several hours to develop. For a mild sprain, swelling could last several days; for severe sprains, swelling normally lasts longer until the injury heals.
When someone experiences a fall, their body releases a natural stress response, known as adrenaline, which can temporarily mask pain and other symptoms. An elderly person might initially feel fine and able to move around after a fall, only to experience significant pain and stiffness several hours or days later once the adrenaline has worn off.
Some injuries may involve internal swelling and inflammation that develops progressively. A minor bump to the head may not hurt immediately, but swelling of brain tissue can develop over 24-72 hours15, leading to increasingly severe symptoms.
Some internal injuries, such as bleeding between the brain and skull, can develop slowly.16 This is especially common in elderly people and those taking blood thinning medication. A small blood vessel may bleed slowly over days or weeks, gradually building pressure in the skull.
Medical professionals recommend monitoring an elderly person for at least 7-10 days following a fall, even if they initially appear uninjured. During this time, you could keep a symptom journal to track changes and look out for:
1-24 hours after a fall:
Changes in energy levels
Difficulty with movements that were initially possible after the fall
Headaches that appear later in the day
Increasing pain or stiffness
Nausea or vomiting
Swelling that develops or worsens
2-3 days after a fall:
Bruising that appears or darkens (although this is normal, monitor the extent)
Changes in sleep patterns
Increasing difficulty with daily activities
New areas of pain or discomfort
Persistent headaches
Worsening pain, rather than improvement
4-10 days after a fall:
Any new symptoms that develop
Confusion or memory problems
Loss of appetite
Mood changes or irritability
Ongoing fatigue or weakness
Persistent or worsening headaches
Please note: This is a guide only and is not medical advice. If you’re concerned about your loved one, seek professional medical advice immediately.
Check thoroughly for injuries before helping the person up – take time to assess how they feel and monitor them closely for the next several hours. Keep them warm and comfortable.
Continue closely monitoring the person and don’t leave them alone. Check on them every 2-3 hours, especially overnight. Encourage gentle movement if they’re able and begin keeping a written record of symptoms. If you have concerns, seek professional medical support.
By day three, symptoms should be stabilising or beginning to improve. If symptoms are worsening, seek professional medical support. Continue monitoring your loved one for new symptoms and try encouraging gentle activity or movement. Apply ice to swelling and keep affected areas elevated when possible.
By this stage, most minor fall injuries should be noticeably improving; lack of improvement suggests professional medical support is required. Continue monitoring symptoms, but the frequency of checks can be reduced. Encourage a gradual return to normal daily activities.
Symptoms persisting beyond 10-14 days require professional medical attention to assess for missed injuries or complications. Consider carrying out your own fall prevention assessment to reduce the risk of future falls.
Keeping a daily log of symptoms after a fall for at least 10 days, noting pain level, new symptoms, mobility changes and overall wellbeing is invaluable. It can help you identify worrying patterns, provide crucial information for medical professionals and create a record for a potential care plan if necessary.
Documenting symptoms tracks progression by distinguishing between normal healing and concerning deterioration. It can help identify delayed symptoms and make it easier to spot new symptoms days after a fall, which will result in better medical consultations. Thorough documentation converts vague concerns like “they just don’t seem right” into concrete data like “they’ve been progressively more confused for three days, and their pain has increased from 3/10 to 7/10”. This level of detail can be crucial in getting appropriate medical care.
Knowing your elderly loved one is living alone can be unsettling. You may be worried they’re struggling by themselves, feeling lonely, or might have a fall while they’re alone. There’s also the concern they won’t communicate these feelings to anyone. However, there are ways in which you can help them and enable them to maintain their independence and routines at home.
Elderly sitting services or Elderly Care at Home can provide reassurance in these circumstances. Elderly sitting services are where a volunteer or Care Assistant visits your loved one at home to provide companionship and social interaction. Elderly Care is similar – a trained, professional Carer will provide support to your loved one at home by carrying out various tasks. These services also provide valuable peace of mind that your loved one is receiving support and there’s someone nearby in the event of a fall.
To learn more about our Home Care services and how we can help, find your local Alina Homecare Team.
1. GOV.UK, “Falls: applying All Our Health”, Reviewed 20 October 2025
2. National Institute for Health & Care Excellence, “Falls”, Reviewed 20 October 2025
3. NHS, “Falls”, Reviewed 20 October 2025
4. Public Health England, “Falls and fracture consensus statement”, Reviewed 20 October 2025
5. National Institute for Health & Care Excellence, “Abaloparatide for treating osteoporosis in postmenopausal women: Draft scope”, Reviewed 20 October 2025
6. GOV.UK, “Falls: applying All Our Health”, Reviewed 20 October 2025
7. NHS, “Osteoporosis”, Reviewed 20 October 2025
5. National Institute for Health & Care Excellence, “Falls: assessment and prevention in older people and in people 50 and over at higher risk”, Reviewed 20 October 2025
9. TakingCare, “Elderly people and falls: how healthcare can better support the UK’s ageing population”, Reviewed 20 October 2025
10. Age UK, “Preventing falls”, Reviewed 20 October 2025
11. NHS, “Whiplash”, Reviewed 20 October 2025
12. Data.Gov.UK, “National Hip Fracture Database annual report 2024”, Reviewed 20 October 2025
13. NHS, “Broken hip”, Reviewed 20 October 2025
14. NHS, “Sprains and strains”, Reviewed 20 October 2025
15. Everyday Health, “What is cerebral edema? Symptoms, causes, diagnosis, treatment, and prevention”, Reviewed 20 October 2025
16. NHS, “Subdural haematoma”, Reviewed 20 October 2025
17. NHS Inform, “Minor head injury”, Reviewed 20 October 2025
18. NHS, “Head injury and concussion”, Reviewed 20 October 2025